This article is part of a series of posts outlining the history and impact of research in experimental organisms. The series is developed in collaboration with the GSA Public Communications and Engagement Committee.
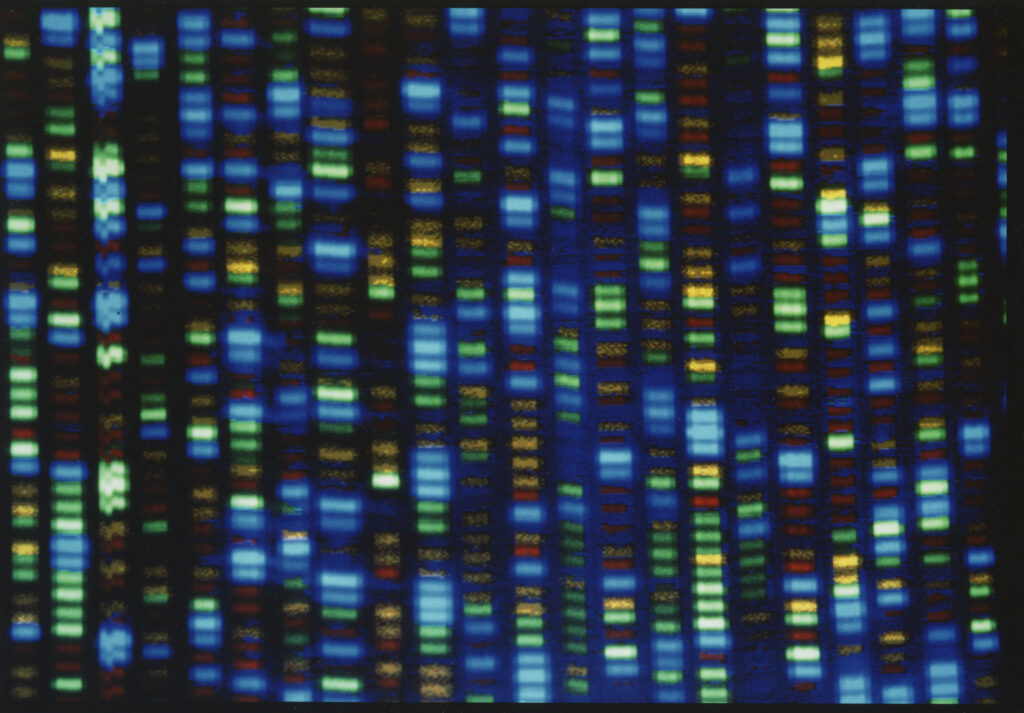
By the time Bertrand Might was six months old, it was clear something was amiss. His muscles weren’t developing normally; he was “jiggly” and had little motor control. As he got older, new symptoms emerged, including seizures, sugars in his urine, and an inability to produce tears. Bertrand’s parents spent countless hours consulting with medical specialists to track down the cause of Bertrand’s illness. In 2010, when he was four years old, the Mights enrolled Bertrand in a clinical trial of a then-novel technology: DNA exome sequencing. Sequencing revealed that he had inherited two different nonfunctional copies of a gene called NGLY1.
With that DNA test, Bertrand became a medical and scientific pioneer—the first patient ever diagnosed with NGLY1 deficiency. But because the disease is so rare, there were no therapies that could cure or treat it at its source; doctors could only try to relieve Bertrand’s symptoms as best they could.
To raise awareness, Bertrand’s dad, Matt Might, published a post on his popular computer science blog detailing the family’s diagnostic odyssey. Over time, the Mights connected with dozens of families also coping with the condition. Interestingly, the collection of symptoms varied quite a bit from case to case,
and genetic sequencing helped a number of families finally put a name to their diseases.
Doctors learned more about the disease with every new patient that came forward. But to really understand how the loss of NGLY1 can cause devastating symptoms throughout the body, scientists would have to take a different path: studying NGLY1’s function in the body at a molecular level. They needed to explore the biochemistry of the protein that NGLY1 encodes, find other molecules that interact with it as it performs its functions, and map out the ripple effects of losing the gene. To capture that level of detail requires controlled studies at a huge scale, something only possible in fast-reproducing research organisms, such as fruit flies and nematode worms.
The not-so-lowly worm
Around the time that doctors were beginning to recognize the clinical effects of NGLY1 deficiency in people, a researcher named Nicolas Lehrbach was making his own surprising discovery about NGLY1, in a different context. Now an assistant professor at Fred Hutchinson Cancer Center, Lehrbach first stumbled across NGLY1 while doing his postdoctoral research at Harvard Medical School.
Lehrbach studies how cells take out their molecular trash, or, more specifically, he studies how cells can compensate when their trash-disposal system isn’t working. When we talk about cellular “trash,” generally that means protein molecules that are damaged, misfolded, or otherwise no longer needed. The cellular machine that breaks down these proteins is called the proteasome. Lehrbach studies the proteasome in the tiny nematode C. elegans—colloquially called “the worm” in biology labs.
“If you think about the fundamental machinery needed by every cell, whether it’s in a human or a worm or a fungus or a plant, there are some basic processes that are simply required for life,” Lehrbach explains. “The underlying molecules that do those jobs are almost the same in any living thing.” The proteasome does one of those essential jobs required by every living animal cell. So by figuring out what molecules keep the proteasome humming along in worms, Lehrbach could also learn something about what makes the proteasome tick in humans.
Worms are inexpensive and quick to breed in the lab—a worm matures from embryo to adult in three days, and each worm produces about 300 offspring.This means that researchers can do thousands of experiments at once looking for rare mutations that affect some aspect of the animal’s development or behavior. Suppose you’re trying to understand how the nervous system develops. First, you would feed the worms a chemical that increases the chances of genetic mutations, and then you’d examine thousands and thousands of mutated worms to find the handful whose nerves didn’t develop properly. By analyzing the genes of those animals, you’d discover which genes contained mutations that caused the defect.
Lehrbach applied this approach to studying proteasome function. He designed a genetic screen to hunt for genes that, when mutated, boost the cell’s production of the proteins that make up the proteasome. “If the proteasome is not working well, one of the ways that our cells can cope with that is just to make more proteasomes to compensate,” Lehrbach says. His experiment revealed that the worm relies on a version of NGLY1 for that process.
“The power of that method is that it doesn’t presuppose any model or hypothesis about what kind of genes are going to be involved,” Lehrbach explains. Rather than choosing a gene and seeing whether it does something important, the researchers can do a wide-ranging search and see what turns up. “I would have never in a thousand years—if I were searching in a more targeted, hypothesis-driven way—I would never have thought the NGLY1 gene would have that role,” he says.
Proteasome failure is a hallmark of various human diseases, including neurodegenerative diseases like Parkinson’s and Alzheimer’s, but Lehrbach wasn’t narrowly focused on pathways involved in disease. The worm studies exemplify how expanding our knowledge of basic cellular processes can lead to unanticipated clinical benefits. “When you have a patient with clinical symptoms, but you want to get back to the molecular mechanism, that’s a really hard puzzle to solve,” Lehrbach says. “That clue from genetics, which really came out of the blue from doing a very open experiment, provided an insight that helped accelerate the process of understanding NGLY1 deficiency.”
Of flies and men
After receiving Bertrand’s genetic diagnosis, the Might family started a foundation, NGLY1.org. Through the foundation, they reached out to geneticist Clement Chow at University of Utah Health for help to uncover more information about how the lack of NGLY1 was making their son ill.
Chow’s lab studies protein misfolding and how the cell deals with incorrectly-folded proteins when they build up in a part of the cell called the endoplasmic reticulum. NGLY1 plays a role in clearing those misfolded proteins, and Chow set out to uncover exactly what that role is.
Using the fruit fly Drosophila in the lab, Chow and his colleagues genetically engineered different flies with different NGLY1 mutants, to see what effect each mutation would have on the fly. Some mutations might completely destroy the NGLY1 protein, while others might just make it weaker or less efficient at doing its job. Flies with mutations in NGLY1 had delays in development, and some died in the larval stage. Others matured to adulthood but still died sooner than normal flies.
Chow also investigated how the loss of NGLY1 changed the expression of other genes. Genes can be turned on or off, meaning they actively produce their protein or they lie idle. They can also be adjusted up or down, like twisting a volume knob on a stereo, so they produce a little more or less protein. Often, these adjustments are managed via biochemical feedback pathways in the cell. NGLY1 removes sugar molecules called glycans from various proteins, and when that function is lost, the excess of glycans alters the activities of those proteins. These changes can have a cascade of effects that lead to changes ingene expression. For instance, there is a protein called Nrf1 whose job is to turn on several genes that make components of the proteasome, to ramp up new production when it detects proteasome failure. It can do this only after NGLY1 removes a glycan from a key building block molecule in the protein, chemically changing its identity. Without NGLY1 there to strip off the glycan, Nrf1 can’t activate those genes, and the cell can no longer compensate for proteasome failure.
By comparing gene expression between healthy flies and those without NGLY1, Chow discovered that losing NGLY1 caused a drop in the level of a protein that helps make a sugar called GlcNAc. Adding and removing GlcNAc from proteins is one key way the cell directs their activity. Currently, GlcNAc is sold over the counter as a supplement. “What’s exciting about this is that patients had already been thinking about using this particular sugar,” Chow says. Because GlcNAc is easy to get, parents of kids with NGLY1 deficiency had tried it at home. “There had been anecdotes that it was providing relief, especially with tear production,” says Chow. When he gave GlcNAc to the mutant flies, they tended to live longer than those that didn’t receive the supplement. A clinical trial of GlcNAc eye drops in kids with NGLY1 deficiency is getting underway at Mayo Clinic to test how well the supplement performs at increasing tear production in these kids who have NGLY1 deficiency.
The GlcNAc discovery in flies not only helped explain how the supplement was helping kids with NGLY1 deficiency, but it was powerful in another way, as well: it validated the fly as a model of how NGLY1 was working in human cells. “That was kind of our first foray into thinking about NGLY1 and what we can do with the fly,” Chow explains.
The next step for the Chow lab was to understand how other genes interact with NGLY1, creating variation in the disease presentation. Among the patients with NGLY1 deficiency, the severity of symptoms ranged widely; for example,the second NGLY1 patient to be identified, Grace Wilsey, learned to crawl, talk, and follow simple directions, skills that Bertrand Might never acquired. Human NGLY1 patients are too few, and too genetically complex, to support clinical studies of genetic interactions that may provide clues to why disease presentation is so variable. Using fruit flies enables researchers to study thousands of animals from genetically controlled populations.
To look at how variants in NGLY1 interacted with other genes in the genome, Chow’s lab turned to the Drosophila Genetic Reference Panel, a collection of fruit fly lines that all carry slightly different genetic changes. The flies were bred from the same original population, so they mostly share the same genome, and each line’s genome sequence is well-documented. By disabling the NGLY1 gene in each different fly population, then documenting the number and severity of the symptoms, they uncovered a gene called NKCC1.
The fruit fly experiments were invaluable to test a large number of genetic interactions in a short period of time, but to fully characterize how the NGLY1 and NKCC1 proteins interact, Chow turned to mice. Experiments in mouse cells grown in the lab revealed exactly how NGLY1 chemically modifies NKCC1 to keep it working properly. “We started out with this very basic tool that fly genetics labs use all the time, which is a genetic screen, and they brought us all the way to thinking of finding defects in mammalian cells in a pretty quick order,” Chow said. “That tells us that the flies are modeling exactly the same thing we see in mice and humans.”
Studying mammalian cells or even human cells grown in a dish in the lab may sound like a more representative model for human disease, but these lab-grown cells can’t perfectly replicate what’s happening in a live animal. To understand the complex interactions between the many genes and proteins over the course of a life cycle, nothing can replace an intact, living animal, even if it’s a miniscule worm or a fruit fly. “There are certain processes, like communication between different types of cells within an organism, that are impossible to model with a layer of cells in a dish, which are all undifferentiated and more or less identical to one another,” Lehrbach says.
And while a worm or a fly can’t exhibit speech delays or intellectual disability, the genes responsible for these issues in people perform largely the same functions on the cellular level in all creatures. “These are mutations in basic housekeeping genes that every organism needs to have functioning,” Chow said. “While their disease may not perfectly match what we see in humans, the cellular process and the biological process is nearly identical in flies and humans, so that makes it a pretty good model for disease.”
For Bertrand Might, genome sequencing revealed the cause of his disease, marking the end of the family’s diagnostic odyssey. At the same time, the diagnosis was only the beginning of a new odyssey: a quest to find a treatment that could compensate for the loss of NGLY1. Sadly, there’s not yet any cure for
NGLY1 deficiency, nor a treatment that directly addresses the genetic cause of the disease. But ongoing research to understand all the different ways that NGLY1 manages important cellular functions is leading to interventions that can lessen the impact of losing NGLY1. While Bertrand himself died in 2020, the research he inspired—including a Precision Medicine Institute at the University of Alabama at Birmingham, which Matt Might directs—aims to someday help other children with NGLY1 deficiency and other rare disorders to live longer, healthier lives.
To learn more about the ways that model research organisms contribute to the study of rare disease, visit any of the links below.
- GENETICS: https://academic.oup.com/genetics/article/214/2/233/5930504
- Undiagnosed Diseases Network: https://undiagnosed.hms.harvard.edu/
- MARRVEL: http://marrvel.org/
- ModelMatcher: https://onlinelibrary.wiley.com/doi/10.1002/humu.24364
- Rare Diseases Models and Mechanisms Network: http://www.rare-diseases-catalyst-network.ca/
- The Jackson Laboratory Rare Disease Translation Center: https://www.jax.org/news-and-insights/2022/December/jax-strives-to-advance-rare-disease-research-andreatment-options
- Zolgensma for Spinal Muscle Atrophy: https://www.pennmedicine.org/news/news-releases/2019/may/zolgensma-based-on-delivery-system-discovered-by-penn-gene-therapy-pioneer
- Zolgensma for Spinal Muscle Atrophy: https://www.sheffieldchildrens.nhs.uk/news/edwards-story-the-world-is-his-oyster-after-gene-therapy-treatment/
- Charcot-Marie-Tooth: https://www.jax.org/news-and-insights/2018/August/kathy-morelli-finding-cures-for-rare-diseases




